Abstract
Introduction
Acute lymphoblastic leukemia (ALL) is a rare disease that affects lymphoblasts derived from lymphoid stem cells and due to the acute nature of this cancer, it is rapidly fatal without treatment (National Cancer Institute, 2016). The average 5-year overall survival (OS) rate was 35% for adult ALL and over 90% of the relapsed or refractory patients eventually die with a median OS of 3-6 months (Kantarjian HM et al. 2010, Bassan and Hoelzer 2011, Forman and Rowe 2013). Allogeneic hematopoietic stem cell transplantation (HSCT) is a potentially curative option for patients with B-cell ALL. Previous studies find that HSCT is associated with high costs and healthcare resource use. However, there is no study examining the allogeneic HSCT costs specifically for the adult ALL patients.
Objective
The aim of this study is to quantify the economic burden of allogeneic HSCT for adult B-cell ALL patients and relapsed adult B-cell ALL patients in the US.
Methods
This was a retrospective cohort study using Truven Health MarketScan® Commercial and Medicare Supplemental Databases. Patients with ≥1 inpatient claims or ≥2 non-diagnostic outpatient claims at least 30 days apart for any ALL diagnosis (ICD-9-CM 204.00-204.02, ICD-10-CM C91.00-C91.02) during 4/1/2009 - 10/31/2016 were extracted. All patients were required to have ≥1 hospitalization with diagnosis-related group in 834-839 on or after the first ALL diagnosis, have ≥1 allogeneic HSCT hospitalization (index date is the admission date for the initial HSCT hospitalization), are ≥18 years old on index date, and have ≥6 months of continuous enrollment prior to index date. Patients with medications for T-Cell ALL during the study period were excluded. Relapsed ALL patients were required to have ≥1 inpatient claims or ≥2 non-diagnostic outpatient claims at least 30 days apart for relapsed ALL diagnosis (ICD9: 204.02, ICD10: C91.02). Patients were followed until the earliest of inpatient death, end of continuous enrollment, or end of the study period (10/31/2016). Outcomes included all-cause and HSCT-related costs and total hospital length of stay (LOS) observed during the index hospitalization, and during 100, 180, or 365 days post-index periods (for the subset of patients with at least 100, 180, or 365 days of continuous enrollment after index date or an inpatient death during that follow-up). The costs for the HSCT-related complications such as graft versus host disease (both acute and chronic), hepatic veno-occlusive disease (VOD), graft failure, serious infections, bronchiolitis obliterans, secondary malignancies, and inpatient death were included, as well as the costs for transplant conditioning regimens during the 14 days before HSCT. Costs were sum of the plan paid amount and out-of-pocket amount in 2016 dollars. All descriptive analyses were conducted for patients with ALL (including both frontline and relapsed ALL) and relapsed ALL, separately.
Results
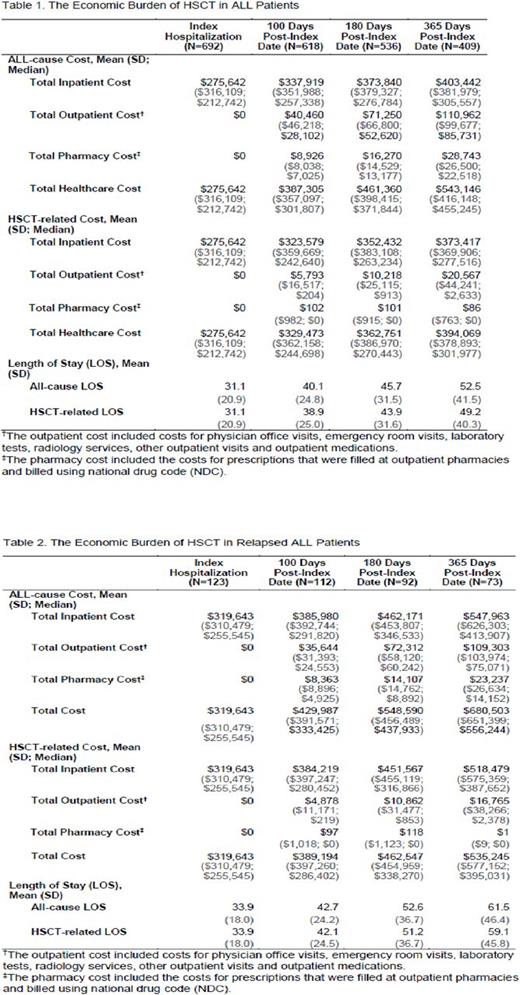
A total of 692 ALL patients (mean age: 45.6; male: 56.1%; mean Charlson comorbidity index: 3.2) were identified. Among all the ALL patients, 123 had relapsed ALL. Among ALL patients, mean (SD; median) costs were $275,642 ($316,109; $212,742) and mean (SD) LOS was 31.1 (20.9) days during the initial HSCT hospitalization (Table 1). During the first year post index, mean (SD; median) all-cause and HSCT-related costs were $543,146 ($416,148; $455,245) and $394,069 ($378,893; $301,977), respectively, with all-cause and HSCT-related mean (SD) LOS of 52.5 (41.5) and 49.2 (40.3) days. Among relapsed ALL patients, mean (SD; median) costs were $319,643 ($310,479; $255,545) during the initial HSCT hospitalization (Table 2). Mean (SD; median) all-cause and HSCT-related costs were $680,503 ($651,399; $556,244) and $535,245 ($577,152; $395,031) during the first year post index. Mean (SD) LOS was 33.9 (18.0) days during the initial HSCT hospitalization and 61.5 (46.4) and 59.1 (45.8) days during the first year post index for all-cause and HSCT-related hospital stays, respectively. The initial HSCT hospitalization accounts for about 47% and 51% of the total costs in the first year after HSCT for ALL and relapsed ALL patients, respectively.
Conclusions
Allogeneic HSCT in ALL is associated with substantial economic burden, especially among relapsed ALL patients. During the first year post HSCT, about half of the total costs occurred during the initial HSCT hospitalization.
Zhang: Amgen Inc.: Employment, Equity Ownership. Cong: Amgen Inc.: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.